Seasonal Affective Disorder (SAD): Complete Guide (Causes, Symptoms, Diagnosis & Treatment)
Seasonal Affective Disorder (SAD) is not just “winter blues.” It is a clinically recognized subtype of major depressive disorder or bipolar disorder that is seasonal in nature, most frequently appearing during the late fall and winter seasons. Since the disorder affects a considerable number of people globally, learning about its causes, symptoms, diagnosis, and scientifically-proven treatments can give patients the power to get support quickly and keep the illness from interfering with their everyday living.
This comprehensive guide breaks down everything you need to know.
What Is Seasonal Affective Disorder (SAD)?
Seasonal Affective Disorder (SAD) is a depressive illness that happens repeatedly and is caused by the change of seasons, usually starting in the fall and lasting through winter. In a few cases, individuals may have a summer-pattern SAD, which means that the symptoms come in the spring or summer.
SAD is a condition in which the body’s internal clock, neurotransmitters, energy, and mood are affected, and these changes are due to exposure to environmental light.
Key Features of SAD
- Changes in symptoms that come and go with the seasons and can be anticipated
- Depressive episodes lasting at least two consecutive years
- Mood, energy, appetite, and sleep are greatly affected
- Symptoms exceeding the limit of a normal seasonal lethargy
According to DSM-5, SAD is considered to be “Major Depressive Disorder with Seasonal Pattern”.
Causes of Seasonal Affective Disorder (Why It Happens)
SAD is not attributable to a single cause. The condition is the outcome of a complicated interplay of biological and environmental factors.
1. Reduced Sunlight Exposure
The leading theory: less sunlight interferes with the body’s internal clock (circadian rhythm). When daylight hours are shorter, the following consequences result:
- Misalignment of sleep–wake cycles
- Lower energy levels
- Mood changes
Residents of areas that are distant from the equator suffer from SAD much more frequently.
2. Serotonin Dysregulation
Serotonin is a neurotransmitter responsible for mood, and its level is reduced in the winter because of:
- Less natural light
- Decreased outdoor activity
- Increased inflammation in susceptible individuals
Serotonin deficiency is very closely related to depressive symptoms.
3. Melatonin Overproduction
Shorter daylight hours lead to an increase in melatonin production, the hormone that helps regulate sleep. Too much melatonin may cause:
- Daytime drowsiness
- Low energy
- Difficulty waking up
- Disrupted sleep cycles
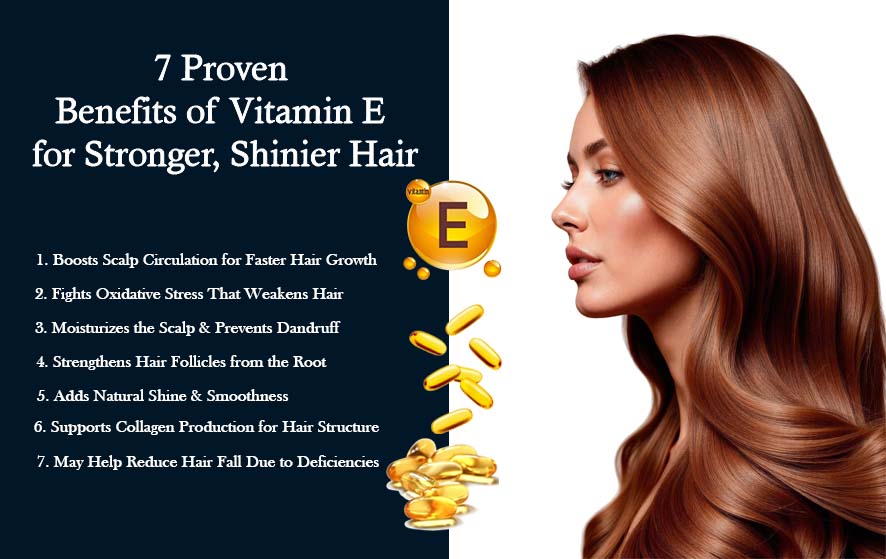
4. Vitamin D Deficiency
Decreased sun exposure significantly diminishes the body’s ability to produce vitamin D naturally. Vitamin D deficiency has been linked to:
- Mood disorders
- Fatigue
- Weakened immune function
5. Genetic & Family History Factors
Individuals carrying genetic predispositions for:
- Depression
- Bipolar disorder
- Seasonal mood changes
are significantly more likely to develop SAD.
6. Psychological & Environmental Stressors
Seasonal affective disorder (SAD) is frequently intensified due to:
- Isolation
- Reduced physical activity
- Holiday-related stress
- Significant life changes
Symptoms of Seasonal Affective Disorder
SAD symptoms overlap with major depression but show strong seasonal patterns.
Winter-Pattern SAD Symptoms
This is the most common form.
Emotional Symptoms
- Persistent sadness or low mood
- Loss of interest in hobbies
- Hopelessness or worthlessness
- Irritability and mood swings
- Increased sensitivity to rejection
Physical & Behavioral Symptoms
- Fatigue and low energy
- Excessive sleeping (hypersomnia)
- Increased appetite, especially for carbs
- Weight gain
- Difficulty concentrating
Atypical Depression Features (Common in SAD)
- Heavy, leaden feeling in limbs (“leaden paralysis”)
- Social withdrawal (“hibernation mode”)
Summer-Pattern SAD Symptoms
Less common and often linked with bipolar disorder.
Emotional Symptoms
- Anxiety
- Restlessness
- Irritability
Physical Symptoms
- Insomnia
- Decreased appetite
- Weight loss
- Heat intolerance
How Is Seasonal Affective Disorder Diagnosed?
Usually, a diagnosis of this kind is assigned by a professional in the field of mental health through the use of the DSM-5 criteria.
Diagnostic Steps Include:
- Nature and behavioral changes monitoring, including sleep and symptoms
- Recognition of seasonal pattern for at least two years
- Exclusion of other medical causes, i.e.:
- Thyroid disorders
- Vitamin D deficiency
- Sleep disorders
4. Determination of functional impairment at work, school, or home
Quite often, your doctor might request:
- Blood tests (thyroid panel, vitamin D levels)
- Psychological questionnaires
- Sleep assessments
Recognition of the disease at an early stage allows for better and even preventive therapy.
Treatment Options for Seasonal Affective Disorder
Seasonal Affective Disorder can be easily cured. In numerous instances, Many people respond well to a combination of therapies.
1. Light Therapy (Phototherapy)
First-line treatment for winter-pattern SAD.
During light therapy, a patient is expected to be near a specially designed 10,000-lux light box for 20–30 minutes every morning. The light helps regulate:
- Circadian rhythm
- Serotonin and melatonin balance
- Mood
- Energy
Improvements can be felt in most cases after 1–2 weeks.
2. Cognitive Behavioral Therapy for SAD (CBT-SAD)
A focused version of cognitive behavioral therapy that addresses the needs of patients:
- Reframe negative thoughts
- Build coping skills
- Modify behaviors that worsen winter depression
CBT-SAD is very effective and has been shown to produce benefits both in the short-term and in the long-term.
3. Medication (Antidepressants)
Examples of selective serotonin reuptake inhibitors (SSRIs) include:
- Sertraline
- Fluoxetine
- Bupropion (FDA-approved for SAD prevention)
may be prescribed for moderate to severe cases.
Medication may be used:
- Seasonally (starting in fall)
- Or year-round for individuals with recurrent episodes
4. Vitamin D Supplementation
Depression associated with seasonal affective disorder (SAD) is often linked to vitamin D deficiency. Your health care provider may suggest:
- Blood testing
- Vitamin D3 supplements
Just as a supplement cannot be the only solution in the case of SAD, however, it could be a support to the other treatment methods.
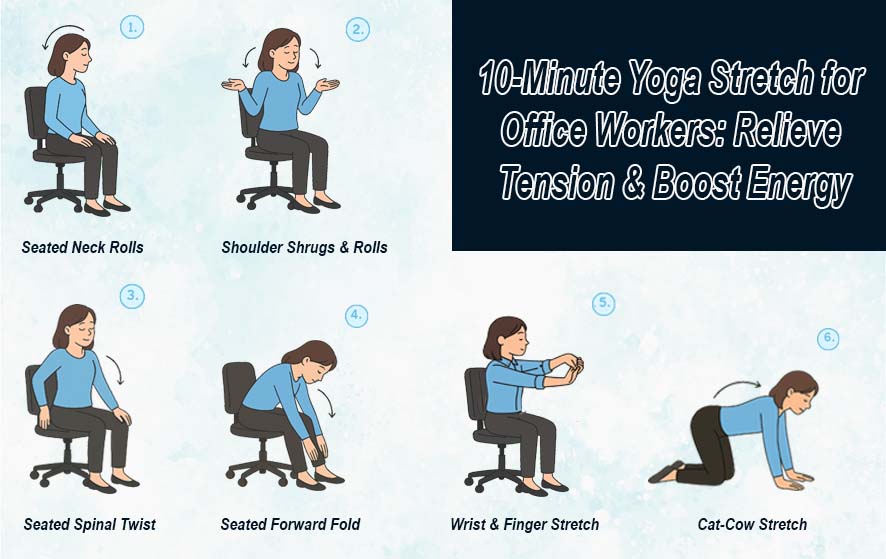
5. Lifestyle & Natural Treatments
Daily outdoor exposure
Just 15–30 minutes can make a big difference in one’s mood and circadian rhythm.
Regular exercise
Boosts serotonin, endorphins, and dopamine.
Healthy sleep schedule
It is also very effective in alleviating symptoms when one goes to bed and wakes up at consistent times.
Nutrient-dense diet
Focus on:
- Omega-3 fatty acids
- Lean proteins
- Fresh produce
- Whole grains
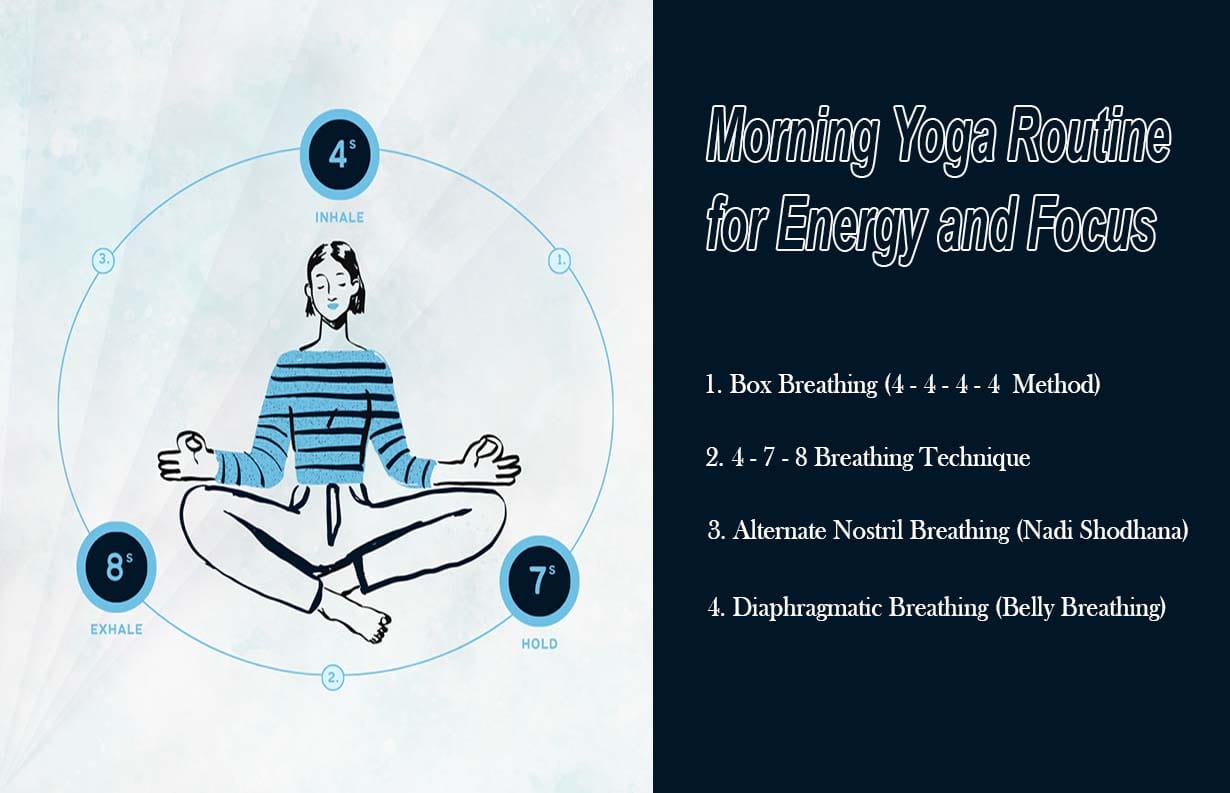
Stress management
Consider:
- Meditation
- Yoga
- Breathing exercises
- Journaling
Prevention: Can You Prevent SAD Before It Starts?
Definitely—if you can predict a seasonal pattern, that is.
Effective Prevention Strategies Include:
- Wear light therapy glasses starting from early fall
- Extend your outdoor activities as much as possible before winter sets in
- Operate a dawn simulator or a daylight alarm clock
- Keep up with your exercise routines no matter what the season is
- If applicable, take bupropion (your doctor will tell you if it’s the case) starting from the fall
- Keep an eye on vitamin D levels
By being on the offensive, you will have fewer and shorter episodes.
When to Seek Professional Help
Reach out to a healthcare provider if you notice:
- Depressive symptoms lasting more than two weeks
- Difficulty functioning at work or home
- Excessive sleep or fatigue
- Thoughts of self-harm (always seek immediate help)
SAD is treatable, and early intervention leads to the best outcomes.