Natural Remedies to Support Breast Cancer Recovery
Note: This article is intended for informational purposes only. It is not a replacement for medical treatment. Always discuss any remedial approach with your oncologist or healthcare provider.

Embracing Healing Beyond Treatment
Recovering from breast cancer is not just about completing treatment — it’s about rebuilding strength, restoring balance, and nourishing the body and mind.
While medical treatments like surgery, chemotherapy, and radiation are essential, natural remedies can gently support your recovery process.
From nutrient-dense foods and healing herbs to relaxation techniques and mindfulness, these holistic approaches can help you regain vitality, reduce side effects, and improve emotional well-being — naturally.
Why Natural Support Matters in Breast Cancer Recovery
Although modern therapies (surgery, hormone therapy, chemo, radiation) form the backbone of treatment, natural and lifestyle-based strategies can still be of great help in several ways:
- They can help manage side effects of treatment (e.g., nausea, fatigue, pain, stress).
- Inflammation and oxidative stress, which may affect recovery and general health over time, are being reduced.
- Supporting immune health, mood, and well-being, which contribute to quality of life and potentially long‐term outcomes.
- They can also facilitate the process of adopting sustainable habits (diet, movement, stress management) that may lower the risk of recurrence or enhance general wellness.
However, a key caveat: natural remedies do not replace standard cancer treatment. According to trusted sources:
“Doctors do not recommend natural and complementary therapies to replace standard treatments for breast cancer.”
And:
“For most of these products, we still do not know whether they work, and studies are required to define whether they are effective and safe and, if so, what dose is required.”
So the goal is supportive care — strengthening your body and mind during recovery, rather than relying on “natural cures.”
Key Natural Remedies and Supportive Strategies
Presented here are the natural ways that have more supporting evidence or are more commonly used to help breast cancer recovery. Every section describes the remedy, the possible benefits, the method of using (or thinking of using), and the safety/interaction notes.
1. Anti-Inflammatory, Antioxidant Foods & Diet
What & how:
- Eating antioxidant-rich food like berries, cruciferous vegetables such as broccoli and cabbage, leafy greens, herbs, and spices (for example, turmeric/curcumin, garlic, ginger) is a very effective way to reduce the inflammatory processes and to detoxify the body from the oxidative damage.
- Omega-3 fatty acids (e.g., those in fatty fish and flaxseeds) not only help to reduce inflammation but can also be a probable source of energy during the recovery phase.
- Dietary fibre coming from plant-based foods is instrumental in the regulation of hormones and overall metabolic health.
Practical tips:
- Eat two or more portions of cruciferous vegetables at least once a week (e.g., Brussels sprouts, broccoli).
- Add turmeric (along with black pepper to enhance absorption) to your cooking or take it as a part of your diet.
- Provide your body with omega‐3s on a daily basis: for example, fatty fish twice a week, or ground flaxseed in a smoothie or yogurt.
- Reduce the intake of processed foods, high sugar foods, and large amounts of red/processed meat since these can lead to inflammation and oxidative stress.
- Keep drinking water and herbal teas (e.g., ginger tea) for an extra benefit.
Safety/notes:
- Breast cancer cannot be cured by a single “super-food”. Diet is a supportive factor in recovery, but it cannot substitute for the treatment.
- In case you are using blood-thinners or you have a surgery planned, some herbal foods/spices (for instance, a high dose of ginger, garlic) may influence bleeding risk — so, always inform your doctor about it.
- The requirements for nutrition are very different after the treatment, especially if you have undergone surgery, chemotherapy, or radiation. The best option is to work with a cancer dietitian.
2. Specific Herbs, Botanicals & Functional Foods
What & evidence:
- Turmeric (curcumin) is often cited for anti‐inflammatory and anti-cancer potential.
- Green tea (catechins like EGCG) may become a source of cancer-fighting agents as it produces very good results in cellular studies.
- Ginger is a safe and effective drug for the relief of nausea that can be caused by chemotherapy, and its anti-inflammatory effect has also been confirmed.
- Flaxseed is one of the most talked about sources of lignans and omega-3s, which are very “hot” substances, especially in hormone-sensitive breast cancer.
- Herbal teas (nettle, chamomile, marigold)are used for stress relief, detox support.
How to include:
- Turmeric: Incorporate it naturally in your diet by making golden milk or if you want to take curcumin supplements, kindly consult your doctor first.
- Green Tea: Take 2-3 cups daily if you can tolerate it.
- Ginger: Make fresh ginger tea or add it to your food; can be supportive for chemo-induced nausea.
- Flaxseed: 1-2 tablespoons of ground flaxseed per day, mixed with yogurt, salad, or smoothie.
- Herbal teas: Use them for relaxation and as a part of your stress-management practice.
Safety/notes:
- Most of the herbal remedies lack strict testing, in aspects such as quality control, dosage, and interactions, in breast cancer recovery.
- As one review states: “We still do not know whether they work, and studies are required… their use merits caution.”
- There are some herbs that can possibly interact with hormone therapy, chemotherapy, or medicines. Make sure that your oncology team always knows about it.
- Do not use herbal products as a substitute for proven medical treatments. For instance, some herbal companies may falsely promote certain products as “cures,” which can be very harmful.
3. Movement, Gentle Exercise & Mind-body Connection
Why it matters:
- Physical activity is crucial to recovery as it helps to bring about several positive changes in the body, such as improving circulation, lymphatic drainage, posture (especially after surgery), muscle strength, mood, and general health.
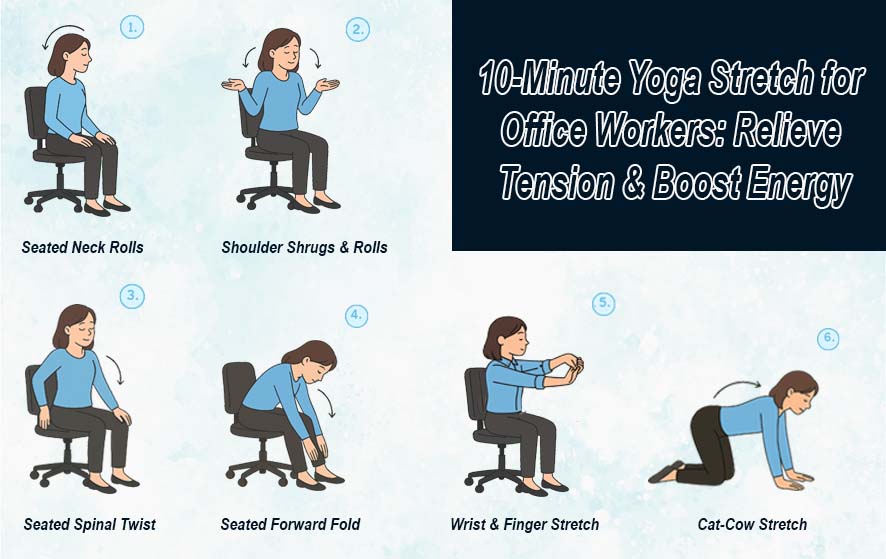
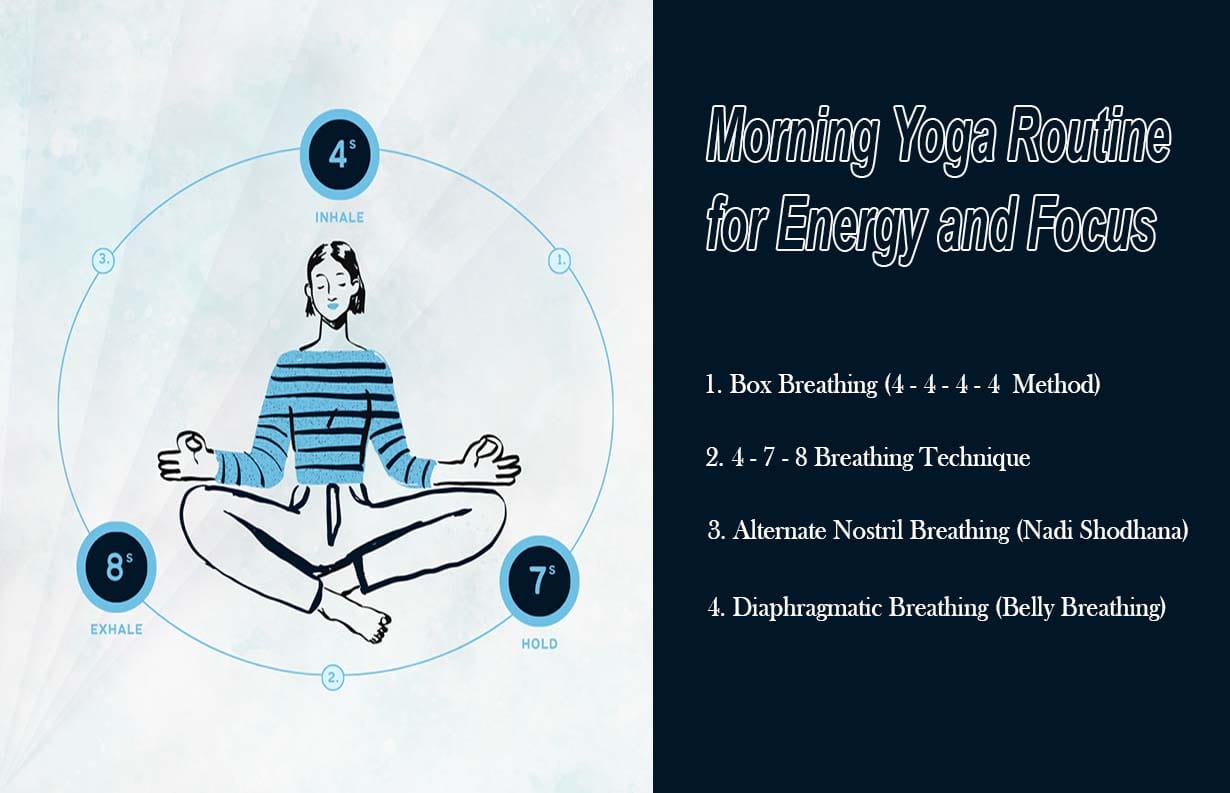
- Mind-body practices such as yoga, tai chi, qi gong, and meditation are effective in alleviating stress, promoting sleep, and enhancing the general well-being of the patient.
Practical recommendations:
- Keep your body in motion for as long as possible with fluid, repetitive movements: e.g., 30 minutes of walking on most days (provided that your doctor has not given you a counter-indication).
- If you have undergone surgery or are receiving radiation/chemo, a physiotherapist or an oncology-exercise specialist should be consulted to ensure that you move safely (particularly the shoulder range of motion).
- Include a comforting method in your daily routine: 10-15 minutes/day of meditation, yoga, or breathing exercises to help mental health.
4. Stress Management & Sleep Hygiene
What to focus on:
- Mental stress and poor sleeping patterns can result in a weakened immune system, and the recovery process will take more time.
- Many of these comforting components can also be a part of an individual’s diet through herbal teas, mindfulness, journaling, and making a sleep routine.
Tips:
- You should personally make sure that you sleep for 7-8 hours at least every night, and also try to keep your bed/wake times consistent.
- Create a wind-down routine: a cup of tea (e.g., chamomile), no use of the screen 1 hour before sleeping, light stretching, or meditation.
- If you find the diagnosis/treatment emotionally too much to handle, you may also think of the support groups or counseling.
5. Lymphatic Support, Detoxification & Post-surgery Care
Why:
- There may be a build-up of lymphatic fluid (lymphedema) or scar tissue after surgery (mastectomy or lumpectomy) and/or radiation. Helping the lymph drainage and detoxification can be of assistance.
- Some natural methods focus on gentle massage, movement (arm exercises), and non-rigid “detox” concepts (although there is little evidence to support them).
Tips:
- Light massage of the surgical area by your own hand (as advised by your physiotherapist).
- If there is lymphedema, then elevation, compression garments (if necessary) should be used under the advice of a specialist.
- Water, fibre, and vegetables are good for the body’s “detox” mechanisms (i.e., liver support rather than radical cleanses).
- Avoid extreme detox diets or “herbal cleanses” that may interfere with healing or medications.
Integrating Natural Support into your Recovery Plan
Step-by-step Integration Guide
- Check with your oncology team: before adding any supplement or major dietary change, ensure it won’t interfere with your treatment or medications.
- Prioritise diet & movement first: foundational changes (whole foods, plant-rich diet, adequate protein, physical activity) give the best “bang for your buck.”
- Add gentle herbs/functional foods: for example, incorporate turmeric/black pepper in meals; drink green tea; add ground flaxseed. Monitor how you feel.
- Support mind and body: schedule 15 minutes of meditation or deep breathing daily; find a gentle yoga or tai chi class suitable for cancer recovery.
- Track your outcomes: keep a journal of side-effects, mood, sleep, fatigue, recovery progress. Share with your healthcare team so adjustments can be made.
- Stay consistent, not extreme: sustainable changes over time work better than drastic overnight shifts.
- Be cautious with claims of “natural cures”: steer clear of any remedy that promises to replace your medical treatment. The science remains provisional.
Safety Considerations & Red Flags
- Always consult your oncologist before starting any supplement or herbal remedy. Examples: high-dose vitamin E, evening primrose oil, some botanicals may have bleeding risks or hormone‐modulating effects.
- Beware of “miracle cure” claims. Some remedies are unsupported by evidence and may delay standard treatment, which can worsen outcomes.
- Quality matters. Supplements and herbs are less strictly regulated than pharmaceuticals; purity, dose and interactions vary.
- Treatment interactions. If you’re on hormone therapy, chemotherapy, targeted therapies, or immunotherapy — natural substances may interfere with their efficacy or metabolism.