Breast Cancer: Causes, Symptoms, Stages, Treatment & Prevention
Breast cancer is still among the top illnesses that affect females all over the globe – and, in a few instances, males as well. The World Health Organization (WHO) reports that over 2.3 million fresh breast cancer cases are detected yearly.
The developments in early detection, precision medicine, and targeted therapies are giving patients the best survival odds ever. However, awareness, prevention, and timely action continue to be the most potent weapons against the disease.
This handbook is an all-inclusive breast cancer overview covering its causes, first signs, stages, treatment options, and prevention tips. Apart from that, you will also get links to the related blogs for a thorough study of the topics.

1. What is Breast Cancer?
Breast cancer is a condition where the cells in the breast tissue grow and divide abnormally, resulting in a lump or tumor. While healthy cells grow, divide, and die in an orderly cycle, cancer cells persistently multiply beyond control. These atypical cells can, after a while, infiltrate nearby tissues or move via the blood and lymphatic system to other locations in the body, which is referred to as metastasis.
Breast cancer has the potential to arise in both females and males; however, it is significantly more frequent in women. The breast consists of lobules (milk-producing glands), ducts (vessels that transport milk to the nipple), and connective tissue (fibrous and fatty tissue that supports the breast). The majority of breast cancers originate from the ducts or lobules.
Benign vs Malignant Tumors
Not all lumps in the breast are cancerous. Frequently, physicians categorize breast swellings into two groups:
● Benign tumors
- Non-cancerous growths that do not invade nearby tissues or spread to other parts of the body.
- Common benign conditions include fibroadenomas and cysts. While they are generally harmless, they might need to be checked or removed if they increase in size or cause discomfort.
- Non-cancerous growths that do not invade nearby tissues or spread to other parts of the body.
- Common benign conditions include fibroadenomas and cysts.
While they are usually harmless, they may require monitoring or removal if they grow or cause discomfort.
● Malignant tumors
- Malignant tumors that have the capability to infiltrate the nearby breast tissue and metastasize to far-away organs (for instance, the lungs, liver, bones, or brain).
- Need treatment by surgery, chemotherapy, radiotherapy, or targeted therapy.
Common Types of Breast Cancer
Different breast cancers vary in their characteristics and treatment responses. The most common types are:
- Ductal Carcinoma In Situ (DCIS): A non-invasive cancer in which the abnormal cells are within the lining of a breast duct, and they haven’t spread outside the duct. Regarded as a very initial stage of breast cancer, with high rates of cure. Usually, a mammogram can find it before any symptoms occur.
- Invasive Ductal Carcinoma (IDC): The most common type of breast cancer which is responsible for about 80% of all cases. Begins in the milk ducts and extends to the adjacent breast tissue. Eventually, if it is not removed early, it can reach the lymph nodes and other organs.
- Invasive Lobular Carcinoma (ILC): The cancer starts gradually in the lobules, the milk-making parts of the breast, and later goes to nearby breast tissue. It is usually difficult to find in a mammogram since it is a single-file pattern growth that doesn’t form a lump.
- Triple-Negative Breast Cancer (TNBC): It is characterized by a lack of estrogen receptors (ER), progesterone receptors (PR), and HER2 protein. The cancer becomes more aggressive and is more difficult to manage with treatments such as hormonal or HER2-targeted therapies. This type of cancer is known to be more prevalent in younger women as well as in some ethnic groups.
- HER2-Positive (HER2+) Breast Cancer: The cancer is caused by excessive production of the HER2 protein that helps cancer cells to grow rapidly. Such tumors have a tendency to get bigger and metastasize fast, but usually, they are responsive to targeted therapies.
It is very important to identify the precise breast cancer type in order to devise a customized treatment plan. In case you have cancer, your doctor should give you the details of your pathology report that describes the tumor type, hormone receptor status, and HER2 status.
For a more detailed explanation of each type, read: Types of Breast Cancer Explained.
2. Causes & Risk Factors of Breast Cancer
Breast cancer is a disease that is not caused by a single factor. It is often a mix of genetic, lifestyle, and environmental factors. Women who have a family history of breast cancer or inherited mutations (like BRCA1/BRCA2) are more likely to develop the disease.
Knowing these risk factors alone does not guarantee that you will get breast cancer; however, it can make it easier for you to take a few preventive measures and recognize it earlier. Some lifestyle factors, such as being overweight, drinking alcohol, not exercising, and being exposed to radiation, can also raise the chances of breast cancer.
Genetic Factors
In some cases, a person may be born (genetically) with changes (mutations) in specific genes that will put him/her at extremely high risk. The most well-known are:
● BRCA1 and BRCA2 mutations
- These tumor-suppressor genes normally function in a way that helps the body to repair the damaged DNA.
- If they are mutated, they lose this capability, giving room for the uncontrolled cells to thrive.
- BRCA mutations can lead to up to 65–80% of the lifetime risk of breast cancer in women carrying them.
- These mutations not only increase the risk of breast cancer but also that of ovarian cancer. In a few instances, the mutations may also lead to pancreatic cancer.
Other inherited gene mutations: The changes in the genes TP53, CHEK2, PTEN, and PALB2 are among the mutations of breast cancer-related genes that are not common and are only linked to the increase of breast cancer risk.
Family history: The risk is increased in a person whose mother, sister, or daughter had breast or ovarian cancer, that is, a first-degree relative, especially when the diagnosis was made before the age of 50 years. Moreover, the probability is higher that the risk will be even more if a larger number of family members have been affected by this disease.
In a case where your family has a history of a particular disease, genetic counseling along with testing can be the key to preventive measures.
Hormonal Factors
Hormones impact the growth of breast cells, and in general, keeping a certain hormone, especially Estrogen, for a very long time would raise the risk eventually.
- Early menstruation (before age 12): Exposes the body to estrogen for a longer time.
- Late menopause (after age 55): Adds several years of estrogen exposure to one’s life.
- Use of hormone replacement therapy (HRT) for a long time: The main source of breast cancer risk is the combined estrogen-progesterone therapy after menopause. If used for 5+ years, breast cancer risk is raised.
- First pregnancy after age 30 or never having children: The breast tissue is less mature and more sensitive to the effects of hormones with time.
Lifestyle & Environmental Factors
Other Medical Conditions
Several risk factors are under your control. You can manage the risk by making changes in your lifestyle.
- Lack of physical activity: A sedentary lifestyle can cause a person to become overweight and hormones to go out of balance. The reason that exercise is good for you is that it helps to regulate your estrogen and insulin levels.
- Unhealthy diet & obesity: Diets rich in processed foods, refined sugars, and unhealthy fats not only make people obese but also can lead to systemic inflammation and hormone imbalance. Obesity after menopause stimulates cancer growth by elevating estrogen levels.
- Alcohol consumption: Even minimal amounts can elevate the risk of breast cancer, and the risk goes up with the increase in alcohol consumption. Alcohol can contribute to high estrogen levels and kill the genetic material in cells.
- Age & Gender: The most hazardous characteristic for breast cancer is femininity; more than 99% of breast cancers occur in women; however, men are not excluded from this disease.
- Age: The likelihood of breast cancer will be escalated to a great extent after the age of 40; hence, the majority of women’s cases are diagnosed after 50 years of age.
- Dense breast tissue: Confuses the detection of tumors with mammograms and is also a source of danger.
- Breast disease in the past: Some benign conditions, like atypical hyperplasia or lobular carcinoma in situ (LCIS), not only increase the risk of breast cancer later but also provide a greater chance of occurrence in the future.
3. Early Signs & Symptoms
Early breast cancer can be a silent foe, presenting no symptoms in many cases. Due to this nature, regular screenings form the first line of defense and are absolutely essential. The list of common warning signs that the body may show also includes a lump found in the breast, unexplained changes in size or shape, skin dimpling, nipple discharge or even swelling in the area under the arm. It is through early identification of these symptoms that seeking medical help promptly becomes possible, thus opening the door to better treatment results.
1. Common Early Symptoms
A lump or thickening in the breast or underarm. The most noticeable sign of the disease is usually experienced during self-examination or during a standard check-up. They might be hard, non-painful, and have an uneven shape, however, some lumps might also be soft and sensitive. No lump is cancer, but a doctor should always verify them. Change in breast size or shape
- Change in breast size or shape: One breast being visibly bigger or smaller than the other. Mysterious bulging or reduction of size that is not related to changes in the menstrual cycle.
- Dimpling or puckering of the skin: The skin might look pitted, similar to the surface of an orange (peau d’orange). Resulting from a hidden tumor that was dragging the skin.
- Nipple inversion or changes: One of the symptoms that occurs with a breast tumor is the nipple turning inward (if it used to be protruding outside). A sudden change from nipple protrusion to retraction of only one breast can be an early indication of breast cancer.
- Nipple discharge: If the discharge is bloody, clear, or happens without squeezing, it is the most worrying type of discharge. The discharge that has a milky appearance and is not related to breastfeeding should be checked as well.
- Persistent breast pain: Persistent pain or irritation at a specific spot on the breast or in the armpit. Generally, breast tumors do not cause pain, yet the cause of pain must always be clarified.
2. Less Common but Important Signs
Redness, rash, or scaling of the breast skin or nipple: These symptoms may look similar to eczema or infection, however, they can indicate inflammatory breast cancer, a severe but rare type.
Swelling in part or all of the breast: Swelling can happen without a lump that can be felt. Usually, skin thickening or warmth is also present.
Changes in skin texture: The area may be thickened or hardened that is localized.
Unexplained bruising without injury: Enlarged lymph nodes under the arm or near the collarbone. They can be similar to small, firm lumps that you can feel. Cancer may have gone beyond the breast if the lymph nodes are enlarged.
3. Why You Shouldn’t Ignore Mild or Unusual Symptoms
- Breast cancer is capable of being quiet and not showing any signs in its initial stages – signs may be very mild.
- It is possible the disease will be unrecognizable with a lump, while the skin or nipples would be affected.
- Increased chances of curing make it possible with the help of self-examination, regular mammography, and clinical check-ups.
Should you observe any one of these changes, be sure to arrange a medical visit without delay, even when there is no breast cancer history in your family.
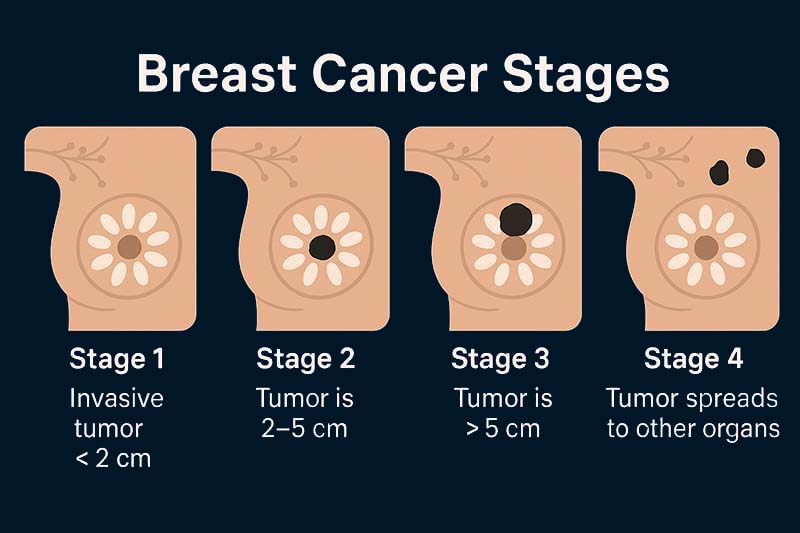
4. Stages of Breast Cancer
Breast cancer is divided into five primary stages (0–4), depending on:
- Tumor size (T)
- Spread to lymph nodes (N)
- Metastasis or spread to other organs (M)
This is the TNM staging system, which is utilized by physicians to decide the most appropriate therapy and estimate the prognosis.
Stage 0: Non-invasive Breast Cancer
Breast cancer is divided into five primary stages (0–4), depending on:
- Tumor size (T)
- Spread to lymph nodes (N)
- Metastasis or spread to other organs (M)
This is the TNM staging system, which is utilized by physicians to decide the most appropriate therapy and estimate the prognosis.
Stage I: Early Invasive Cancer
- Tumor size: 2 cm or less.
- Spread: No lymph node involvement, or tiny clusters of cancer cells in the lymph nodes closest to the tumor.
- Sub-stages:
- Stage IA: Tumor less than or equal to 2 cm with no spread to lymph nodes.
- Stage IB: Either a small tumor or no tumor in the breast, but with a few cancer cells in the lymph nodes.
- Treatment description: The main treatment was surgery (lumpectomy or mastectomy). Usually, surgery is followed by radiation. In addition, there may be hormone or targeted therapy.
Stage II: Growing Tumor, Possible Lymph Node Involvement
Tumor size: 2–5 cm, with spread up to 3 lymph nodes or without lymph node spread.
Sub-stages:
- Stage IIA: Tumor of 2 cm or less with spread to 1–3 lymph nodes, OR Tumor 2–5 cm with no lymph node spread.
- Stage IIB: Tumor 2–5 cm with spread to 1–3 lymph nodes, OR Tumor> 5 cm with no lymph node spread.
Prognosis: Continued to be very treatable, but the risk of recurrence is increased if not treated early.
Stage III: Locally Advanced Breast Cancer
Cancer has gone through the lymph nodes or tissues around the breast, but it has not been found in organs far away.
Sub-stages:
- Stage IIIA: The tumor can be of any size with cancer in 4-9 lymph nodes, or a large tumor with limited local spread.
- Stage IIIB: The tumor has either penetrated the chest wall or skin and is likely to cause ulceration or skin changes (peau d’orange).
- Stage IIIC: Cancer in 10 or more lymph nodes, or spread to lymph nodes above or below the collarbone.
- Treatment used: Surgery, chemotherapy, radiation, hormone therapy, and targeted drugs, all in combination.
Stage IV: Metastatic Breast Cancer
The cancer has spread to distant organs, such as:
- Bones
- Liver
- Lungs
- Brain
The symptoms are diverse depending on the metastasis location, and can be bone pain, breathing problems, jaundice, or neurological symptoms.
Prognosis: Stage IV is still terminal; however, therapy may alleviate symptoms, retard progression, and elevate quality of life.
Understanding your stage helps you make informed treatment decisions. For an easy visual breakdown, see our Breast Cancer Stages Explained Simply chart.
Breast Cancer Stages Explained Simply chart
5. Diagnosis & Screening
One of the most powerful methods to increase the breast cancer survival rate is early identification. Through regular screening, it is possible to find the cancer at the stage when symptoms are not yet evident, and in most cases, this is the stage at which the cancer is the easiest to treat.
Physicians rely on patient self-examination, medical examination, and imaging procedures to locate the abnormalities.
A. Breast Self-Examination (BSE)
Purpose: It is a process that helps you to get acquainted with the usual appearance and texture of your breasts so that you can notice the changes at an early stage.
Best time: 3–5 days after your period starts (when breasts are least tender).
How to perform:
- Visual Check – With your arms down and then up, stand in front of a mirror and check for any changes in the size, shape, skin, or nipple position of the breasts.
- Palpation Standing – While in the shower, use the finger pads of the hand to feel for lumps.
- Palpation Lying Down – Put a pillow under one shoulder and touch the other breast with your hand in circular motions, taking off the area around the breast and armpit.
Warning signs to report: Lumps, thickened tissue, skin dimpling, nipple inversion, discharge (especially bloody), or redness/swelling.
B. Clinical Breast Examination (CBE)
- Performed by: A healthcare professional who is skilled in the procedure.
- Frequency:
- 20–39-year-olds: Every 3 years.
- 40+ year-olds: Annually, together with other screenings.
- Purpose: The detection of lumps or changes that the pe
C. Imaging Tests
1. Mammogram – The Gold Standard
- What it is: The breast is imaged using a low-dose X-ray.
- Purpose: Find tumors or calcifications that can be even smaller than a finger grain of sand.
- When to start (average risk): From the age of 40, yearly.
- High risk: It may be a 30-year starting point, the doctor will decide.
- Advantages: It is able to uncover cancer several years before the onset of symptoms.
- Limitations: There is a possibility that it is less accurate in dense breast tissue and, consequently, additional imaging is required.
2. Breast Ultrasound
- What it is: Uses sound waves to generate pictures of breast tissue.
- Purpose: Primarily employed along with a mammogram as a diagnostic tool to help identify if the lump is a solid tumor or a cyst filled with fluid.
- Best for: Women who are under 40 or those having dense breast tissue.
3. Magnetic Resonance Imaging (MRI)
- What it is: Breast MRI is a detailed breast imaging procedure that involves the use of magnetic fields and radio waves.
- Purpose: The test is generally suggested for patients who are at high risk or to find out how far cancer has spread after diagnosis.
- Advantage: Very sensitive; the technology allows the detection of tumors that cannot be detected by a mammogram.
D. Biopsy – Confirming the Diagnosis
- When imaging raises suspicion of an abnormality, a biopsy is done to take a tissue sample for laboratory analysis.
The procedures are:
- Fine-needle aspiration (FNA): A thin needle is used to extract cells or fluid.
- Core needle biopsy: Extracts a small tissue sample in the shape of a cylinder.
- Surgical biopsy: Partially or completely removes a lump.
Pathology results determine:
- The cells’ nature, whether they are cancerous or not.
- The cancer type (ductal, lobular, etc.).
- The hormone receptor status (ER/PR) and HER2 status, which are used to direct treatment besides
E. Breast Cancer Screening Guidelines at a Glance
| Age Group | Screening Recommendation | Purpose |
| 20–39 | Monthly self-exam + clinical exam every 3 years | Familiarity with normal breast tissue |
| 40+ | Annual mammogram + annual clinical exam | Early cancer detection |
| High risk | MRI + mammogram annually (starting at 30 or earlier) | Detect cancer at earliest stage possible |
Screening schedules may vary based on family history, genetic mutations (like BRCA1/BRCA2), and other risk factors. Always consult your healthcare provider for a personalized screening plan.
6. Treatment Options
The approach to breast cancer is extremely individualized, varying with the kind, progression, hormone receptor profile, HER2 status, and the general condition of the patient.
Usually, patients undergo a mix of treatments to get the optimum result.
The principal treatment types are surgery, radiotherapy, drug therapy, hormone therapy, and targeted or immune-based therapies.
A. Surgery
Surgery is a process of removing breast cancer physically from the breast, and sometimes, the lymph nodes that are close to the area.
1. Lumpectomy (Breast-Conserving Surgery)
- The tumor and a small margin of normal tissue around it are removed.
- The main aim is to make sure the tumor is completely removed while retaining as much as possible.
- Typically, the patient receives Radiation therapy to lower the chances of recurrence.
- The most appropriate treatment option for Breast cancer of the initial stage is when the tumor is small and localized.
2. Mastectomy
What it is: The complete removal of the breast.
Variations:
- Simple (Total) Mastectomy: The removal of the breast tissue only.
- Modified Radical Mastectomy: The removal of breast tissue and some of the lymph nodes in the underarm area.
- Skin- or Nipple-Sparing Mastectomy: The removal of the breast, leaving skin and/or nipple for the patient to have a reconstruction.
Such a recommendation could be made in the instance where the tumors are huge, numerous, or in conditions with a high hereditary risk (BRCA mutations).
3. Lymph Node Surgery
- Sentinel Lymph Node Biopsy: Identifies the initial lymph nodes that are the most probable sites of cancer metastasis.
- Axillary Lymph Node Dissection: Surgically extracts several lymph nodes in case cancer has spread radially into them.
B. Radiation Therapy
- Purpose: Essentially, the very energetic X-rays or proton rays are used to destroy cancer cells that have been left after the surgery.
- When used: Generally after a lumpectomy; however, postoperative radiation therapy might be applied after a mastectomy when cancer has invaded the lymph nodes.
- Types: External Beam Radiation – The most frequent method; directs radiation from the outside of the body on the breast or chest area. Brachytherapy – Inserts small radioactive seeds or pellets directly in breast tissue for short-term treatment.
- Duration: Normally, treatments are done every day for 3 to 6 weeks.
- Side effects: Side effects include tiredness, skin redness, and minor swelling (which is usually temporary).
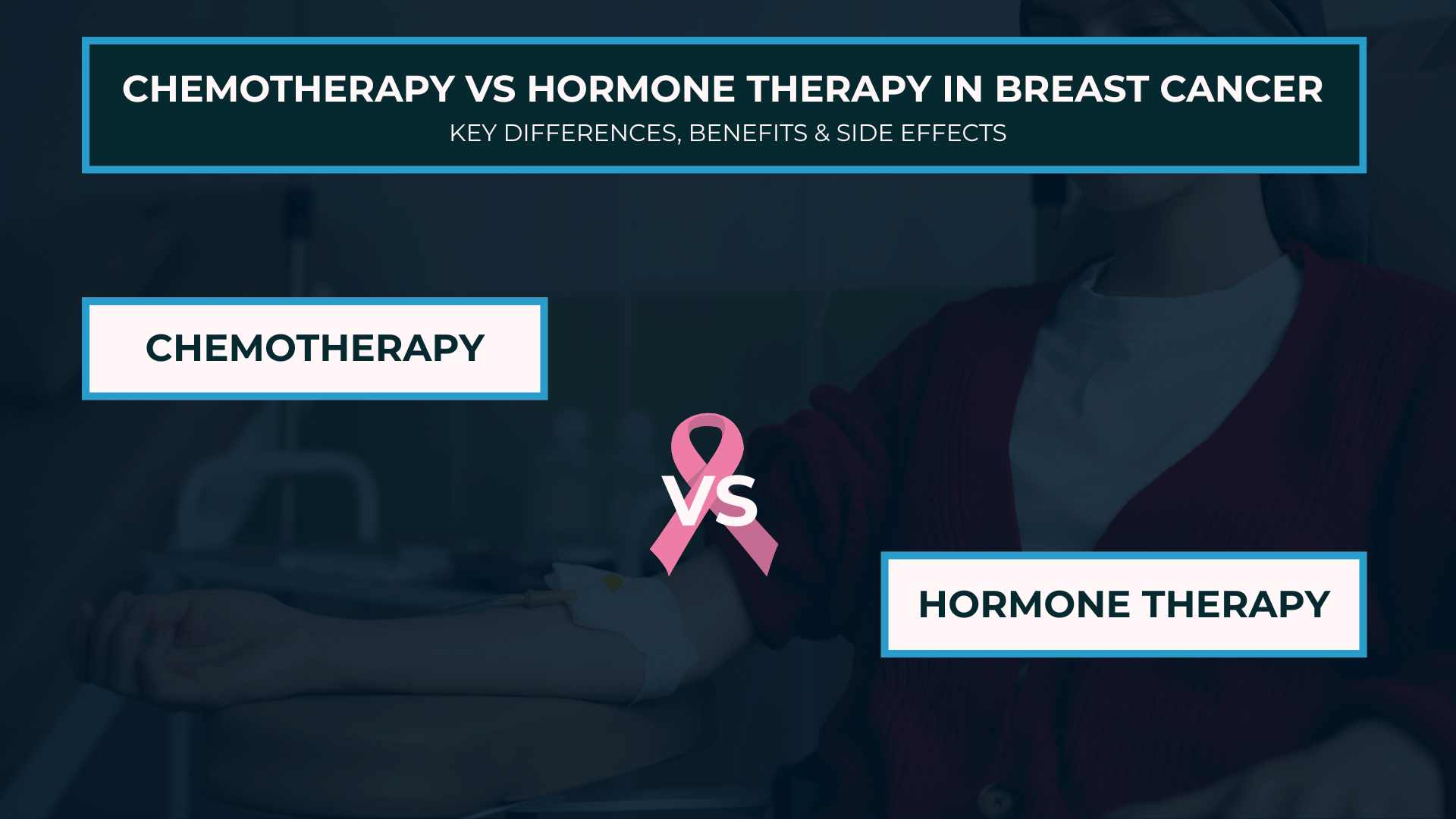
C. Chemotherapy
- What it is: The procedure involves the use of extremely strong drugs to destroy cancer cells that multiply rapidly all over the body.
- When it is administered: Before surgery (neoadjuvant) – The tumors are reduced in size for an easier surgery. After surgery (adjuvant), the risk of recurrence is lowered. For advanced cancer, the progression of the disease is delayed.
- Side effects: Loss of hair, vomiting, tiredness, lowered resistance to infection, though most are temporary and can be controlled
D. Hormone Therapy
- Purpose: Endocrine therapy is aimed at HR+ breast cancer, such as those types where the cells are set to grow if exposed to estrogen or progesterone, and works in a manner to prevent such growth.
- How it works: The therapy utilises medication that either ceases the production of hormones by the body or willfully interferes with their effects. Aromatase inhibitors help the body of a postmenopausal woman produce less estrogen.
- Duration: It is quite common that the treatment is recommended to be between 5 and 10 years with the purpose of reducing the risk.
- Duration: It is commonly recommended as a treatment for 5-10 years to reduce the chance of the tumor coming back.
E. Targeted Therapy & Immunotherapy
1. Targeted Therapy
- Goal: To destroy cancer cells that have been identified to have a specific molecular markers, while at the same time not harming healthy cells.
- HER2-positive (HER2+) breast cancer is the one where the cancer cells have more than a normal amount of the HER2 protein, which causes their growth. Approximately 15% to 20% of breast cancers are HER2+.
- CDK4/6 inhibitors are used for certain HR+ breast cancers.
2. Immunotherapy
- Goal: Makes use of the patient’s immune system to combat cancer.
- Immunotherapy may be used for triple-negative breast cancer with PD-L1 expression.
F. Supportive & Integrative Therapies
Though it is not a treatment, the supportive care extensively contributes to the upgrading of the patient’s life during the process of the disease:
- Nutritional guidance.
- Rehabilitation after an operation.
- Psycho-social support and therapy.
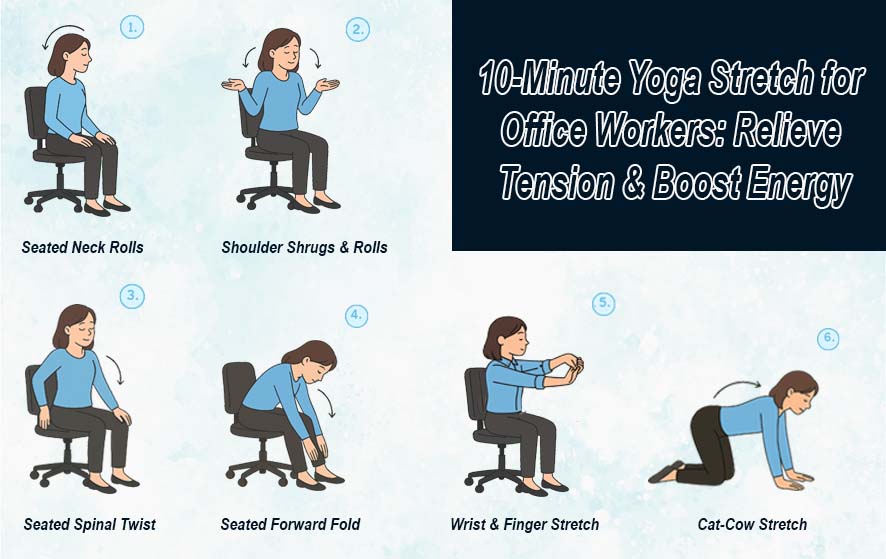
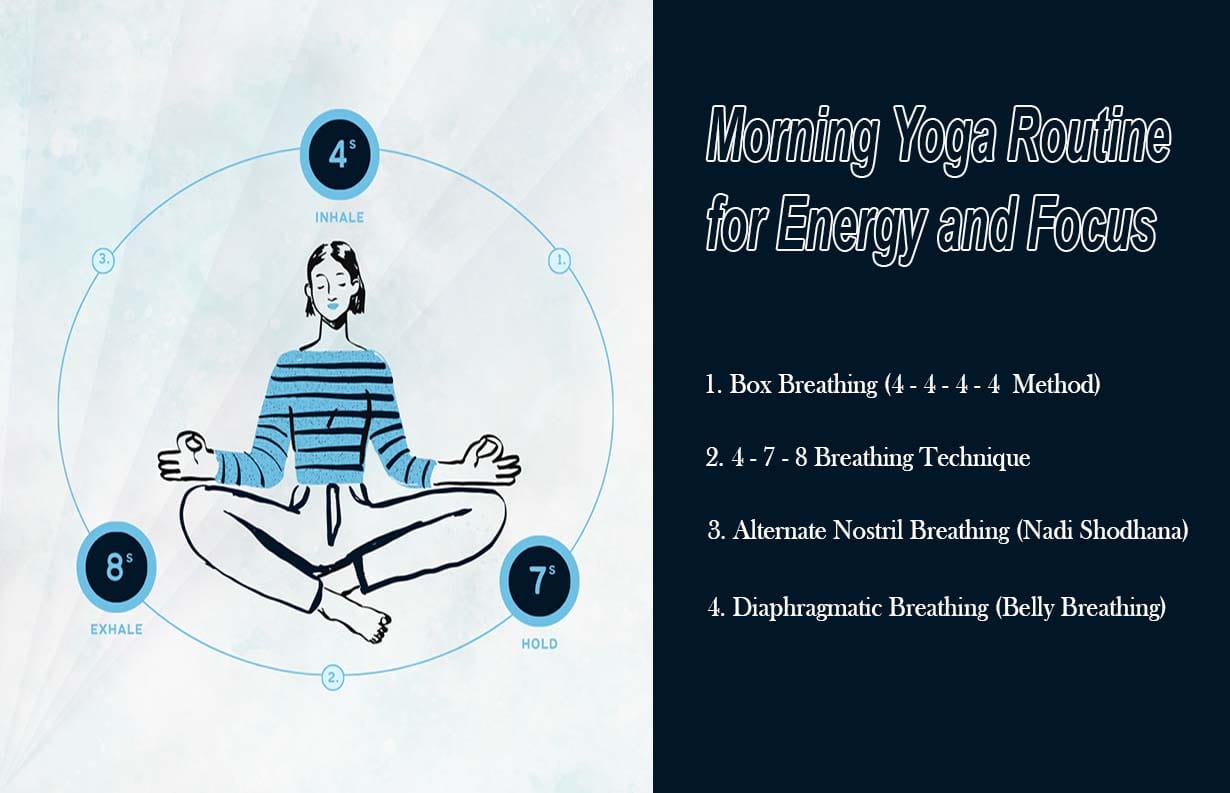
- Light work out and relaxation methods, such as yoga or meditation.
The best treatment plan is personalized, often combining multiple therapies for maximum effectiveness. Patients should discuss all possible options, including clinical trials, with their oncologist.
7. Life During & After Treatment
Life during and after breast cancer treatment can feel like going through a new phase — in your body, your feelings, and your relationships. The courses of each patient are unlike each other, but you will find that there are common issues and ways that can be beneficial to you in handling side effects, regaining energy, and bringing back self-esteem.
- Managing side effects like tiredness,, nausea, and hair loss
- Physical rehabilitation & gentle exercise
- Emotional & mental health support
Joining breast cancer survivor networks
8. Diet & Lifestyle for Breast Cancer Patients
The Nutrition and lifestyle that you make are very important to the body of the patient who has breast cancer, and also to the body after the treatment of
breast cancer. No one food can cure breast cancer. Still, a healthy, anti-inflammatory lifestyle and diet can play a vital part in the body by strengthening it, providing it with various nutrients, and also making the life of the person more comfortable throughout the treatment period.
- Best Foods: Leafy greens, berries, salmon, whole grains
- Foods to Avoid: Processed meats, sugary snacks, alcohol
9. Prevention Tips
These are good tips for breast cancer prevention.
- Maintain a healthy weight
- Exercise regularly
- Limit alcohol intake
- Get regular screenings
Consider genetic counseling if at high risk
10. Breast Cancer Myths vs Facts
- Myth: Only women get breast cancer → Fact: Men can also be affected.
- Myth: A lump always means cancer → Fact: Many lumps are benign.
11. Awareness & Support
- October is Breast Cancer Awareness Month
- Wear pink ribbons, join awareness events, and support research funding
12. Inspirational Survivor Stories
Breast cancer is a tough journey, but many women and men have fought and survived it with courage. Their stories bring inspiration to others going through similar ordeals. Here are a: